Heart Rate Variability: Physiology and Applications
Understanding athletes recovery needs are key to ensuring that the training stimulus is properly planned and assimilated. Given the unique characteristics of each individual, the ability to potentially measure an athlete’s response to training can be key to tailoring training to their characteristics. In this context, one of the most effective and accessible methods to assess individual responses to training is the measurement of resting physiology in terms of heart rate and heart rate variability (HRV) (1, 2).
Heart rate and HRV can be seen as proxies of physiological stress, due to the relationship between stress, the autonomic nervous system, and heart rhythm. In particular, sources of stress (stressors) are disruptions that trigger specific responses as the body tries to maintain a state of balance, called homeostasis. Impulses from the brain and spinal cord to smooth muscles and (among others) the heart is conducted by the autonomic nervous system. Thus, the autonomic nervous system controls and regulates many functions of the body, from the heart beating to respiration, in response to the stressors we face. We typically think of the autonomic nervous system in the context of its two branches, the sympathetic and parasympathetic nervous systems. While the sympathetic nervous system is responsible for stimulating the body’s fight or flight response, the parasympathetic nervous system is mainly responsible for the body’s resting functions (1, 3). Both resting heart rate and HRV are mediated by neurons with parasympathetic and sympathetic origin.
Training is typically the most important stressor we intentionally and consistently apply in order to improve an athlete’s performance. Changes in resting heart rate and HRV can reflect our response to training and other stressors and therefore help us individualize training. The basic physiological mechanism highlighted above, together with the ease of measurement with respect to alternative pathways activated in response to stress (e.g., hormonal), make HRV a useful parameter in the context of quantifying individual recovery needs and potentially optimizing performance – when properly utilized.
The Physiology of HRV
In this section, we cover in more detail the physiological underpinnings of HRV. Heart rhythm (resting heart rate and HRV) is impacted by the autonomic nervous system’s response to stress. Let’s better define these terms first. When we talk about heart rate, we refer to the number of heartbeats that we can count over a period of time, typically a minute. On the other hand, HRV is a term that refers to ways to summarise in a number the variability between heartbeats because even if we count 60 beasts in a minute, they do not happen exactly every second.
As introduced in the previous section, both your heart rate (number of beats) and your HRV (variations in timing between consecutive beats) are modulated by the autonomic nervous system in response to stress. In particular, the heart has its own pacemaker, meaning that there’s a spot (called a sinoatrial node) that generates electric potentials that initiate contractions, resulting in heartbeats. If you had no other mechanism to modulate heart rhythm, your heart would beat at approximately 100 beats per minute (bpm), due to this pacemaker. This intrinsic firing rate is rather constant (hence ~no variability or HRV is present in this state). On top of this basic mechanism, the heart is innervated by the autonomic nervous system. If you have measured your resting heart rate, you have seen that most likely, it is quite a bit lower than the intrinsic firing rate of 100 bpm. In the general population, anything around 60 or 70 bpm is considered normal, while lower heart rates are common in athletes. This tells us already that at rest, parasympathetic activity is predominant, as heart rate is highly reduced with respect to the intrinsic rate of firing of the sinoatrial node (4).
When we face a stressor, impulses from the brain, starting in the hypothalamus, are sent to (among others) the heart via the autonomic nervous system, using neurotransmitters. The main neurotransmitter of the parasympathetic system is acetylcholine, while the sympathetic system relies mostly on norepinephrine. Thus, when acetylcholine is released, it binds to receptors near the sinoatrial node and slows down the heart rate. This process is quick, with latencies in the order of milliseconds, which means that the parasympathetic system can slow down heart rate almost instantaneously (2, 4), effectively delaying the next heartbeat (and therefore increasing HRV). Due to the timing of parasympathetic activity, which is impacted by respiration, and increased during the exhale, HRV captures information not present in average heart rate alone, highlighting an important difference at the physiological level. We will see later how these differences result in HRV being a more sensitive marker of stress (5, 6).
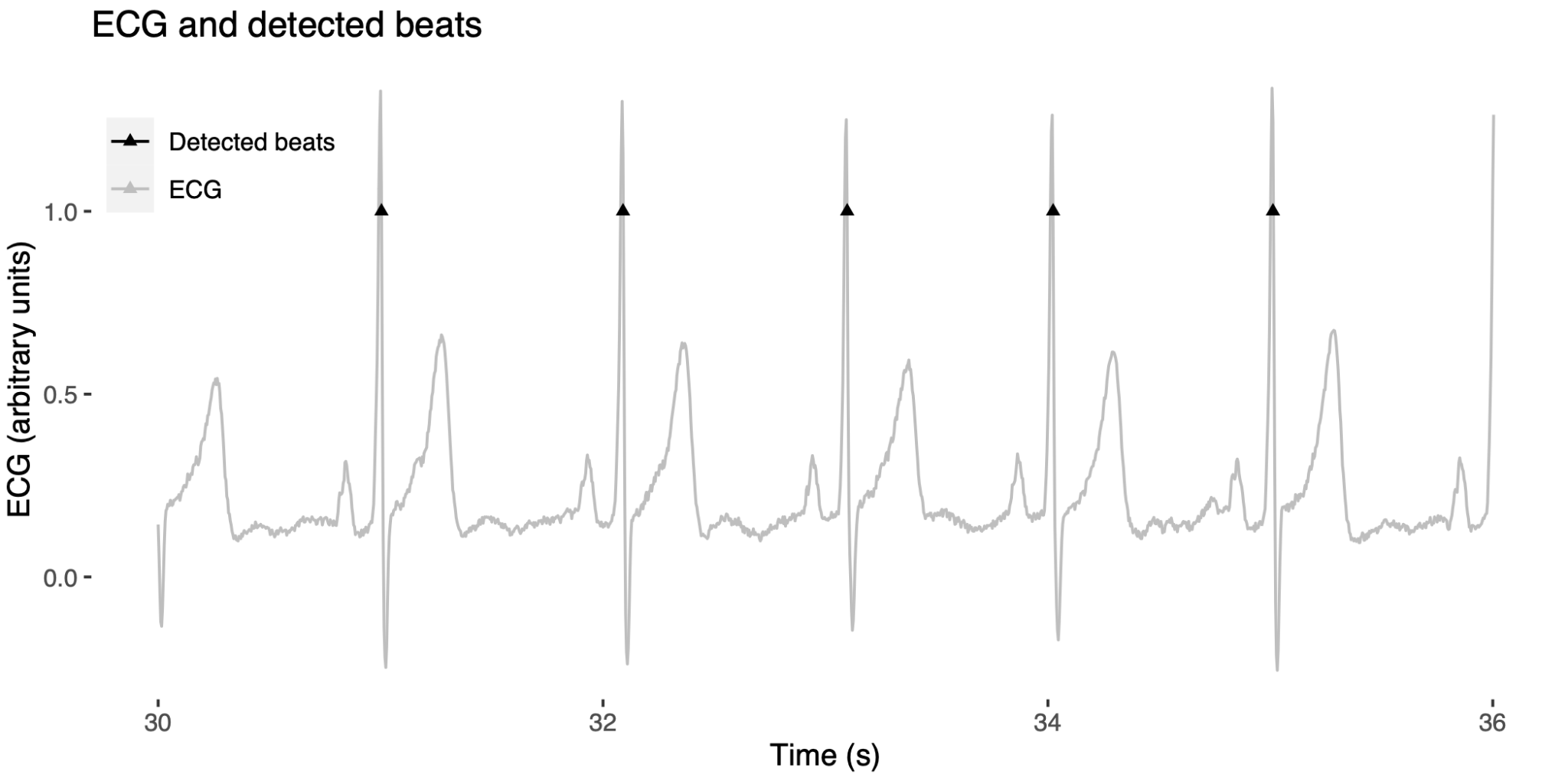
Figure 1 – A few seconds of electrocardiography, showing timing differences between consecutive peaks (RR intervals).
Getting Practical: Data Collection and Interpretation
In the previous sections, we have seen how HRV can be considered a proxy for physiological stress. Given the myriad of apps, sensors, and wearables that promise to measure HRV today, we need to be able to identify the ones that can give us useful insights.
In particular, there are three key steps to make use of HRV data:
- Collecting accurate data
- Collecting meaningful data
- Interpreting the data
Collecting Accurate Data
Technology for HRV measurement at rest is getting better every day. At HRV4Training, we have developed the first camera-based approach to collect HRV data accurately, which has been validated (7), and independently validated (8). Additionally, other devices have been recently validated for either spot checks or night long recordings.
Collecting accurate data means that when we take a measurement, we measure HRV with a degree of accuracy that is similar to reference systems, such as an electrocardiogram (ECG). This boils down to being able to measure the RR intervals correctly (or PP intervals for optical methods). When you pick an app or sensor, the question to ask is the following: is there a validation of this app or sensor showing that when triggering an HRV measurement, the data is equivalent to an ECG (or Polar chest strap)? If there is no data showing this level of accuracy for the device you are interested in, don’t bother.
Here are a few options, including their validations:
The practical implications of these models are instantly evident. If you have …











Responses